-
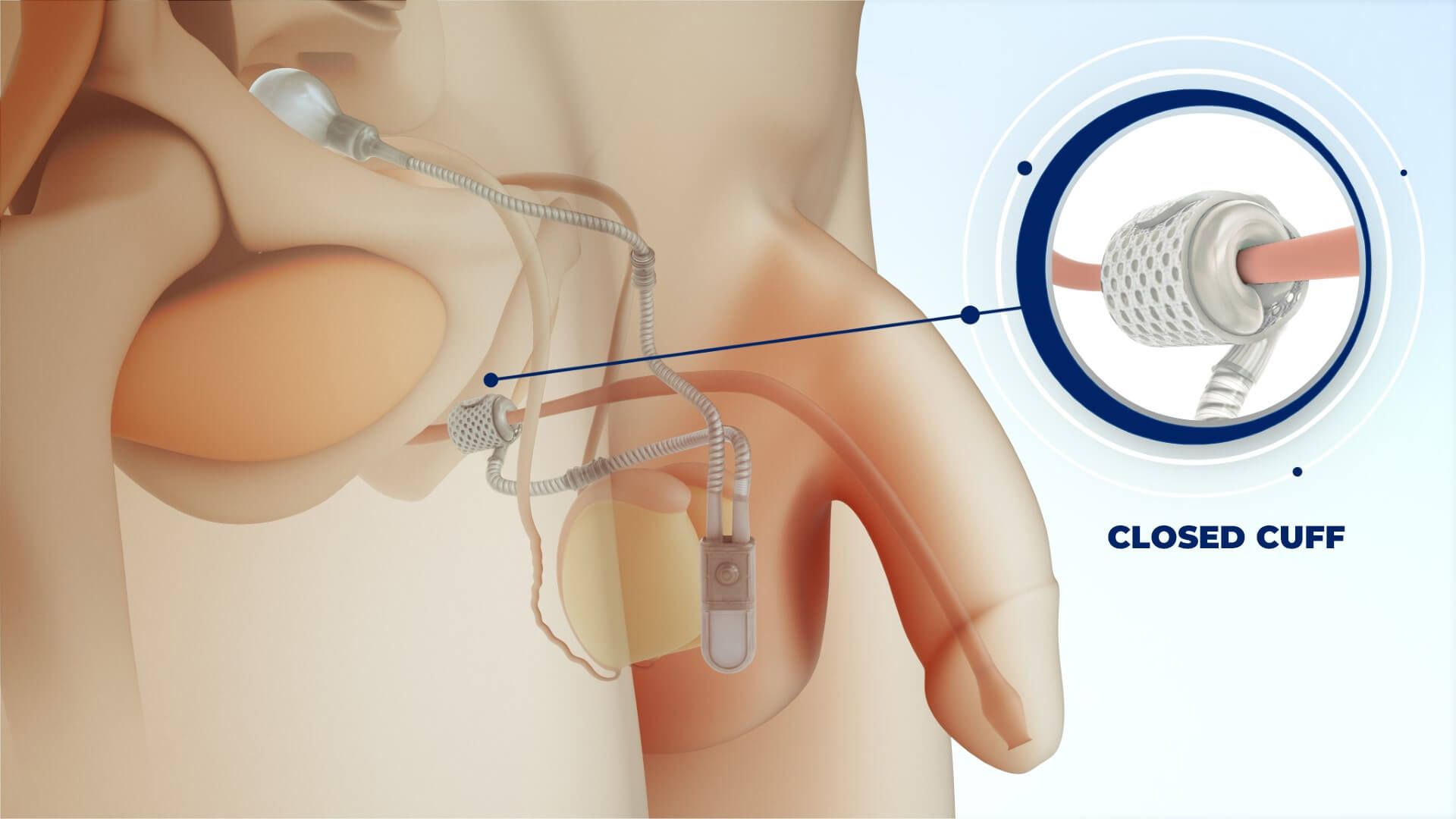
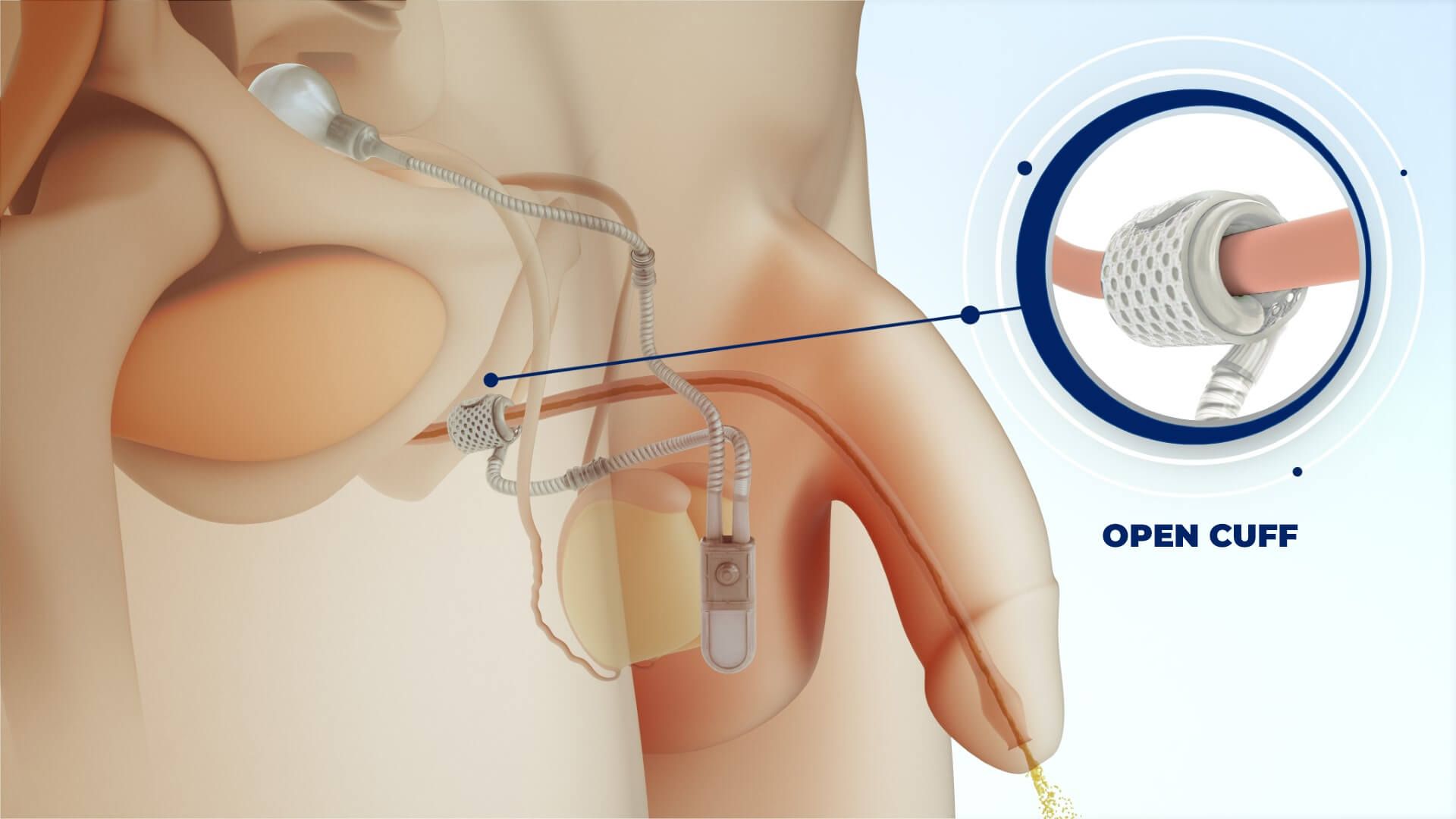
ContiClassic® Artificial Urinary Sphincter is used to treat urinary incontinence due to sphincter deficiency in cases such as incontinence following prostate surgery.6
Pressure Regulating Balloon
We offer five different size of Pressure Regulating Balloon options, each designed to function optimally at a specific pressure level.
New Cuff Sizes
New and diverse occlusive cuff sizes for a surgeon-made fit to the patient’s urethral anatomy.
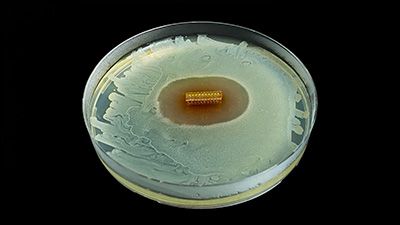
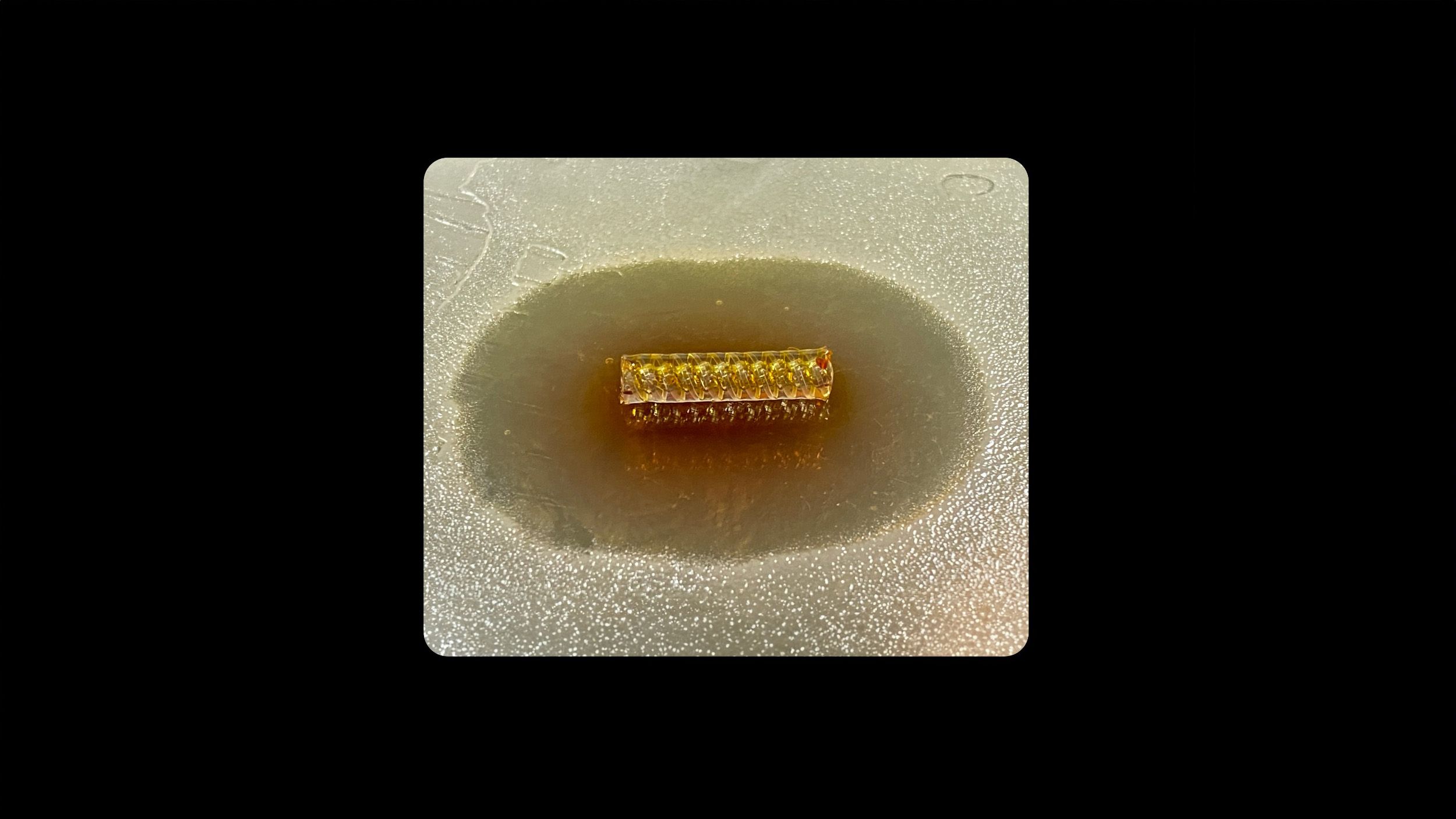
HydroShield™ Coating
ContiClassic® features a hydrophilic coating on all external surfaces, including the pressure regulating balloon, allowing for compatibility with various antibiotics tailored to the patient’s needs.2
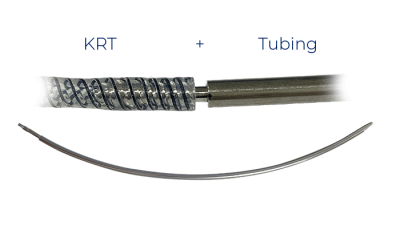
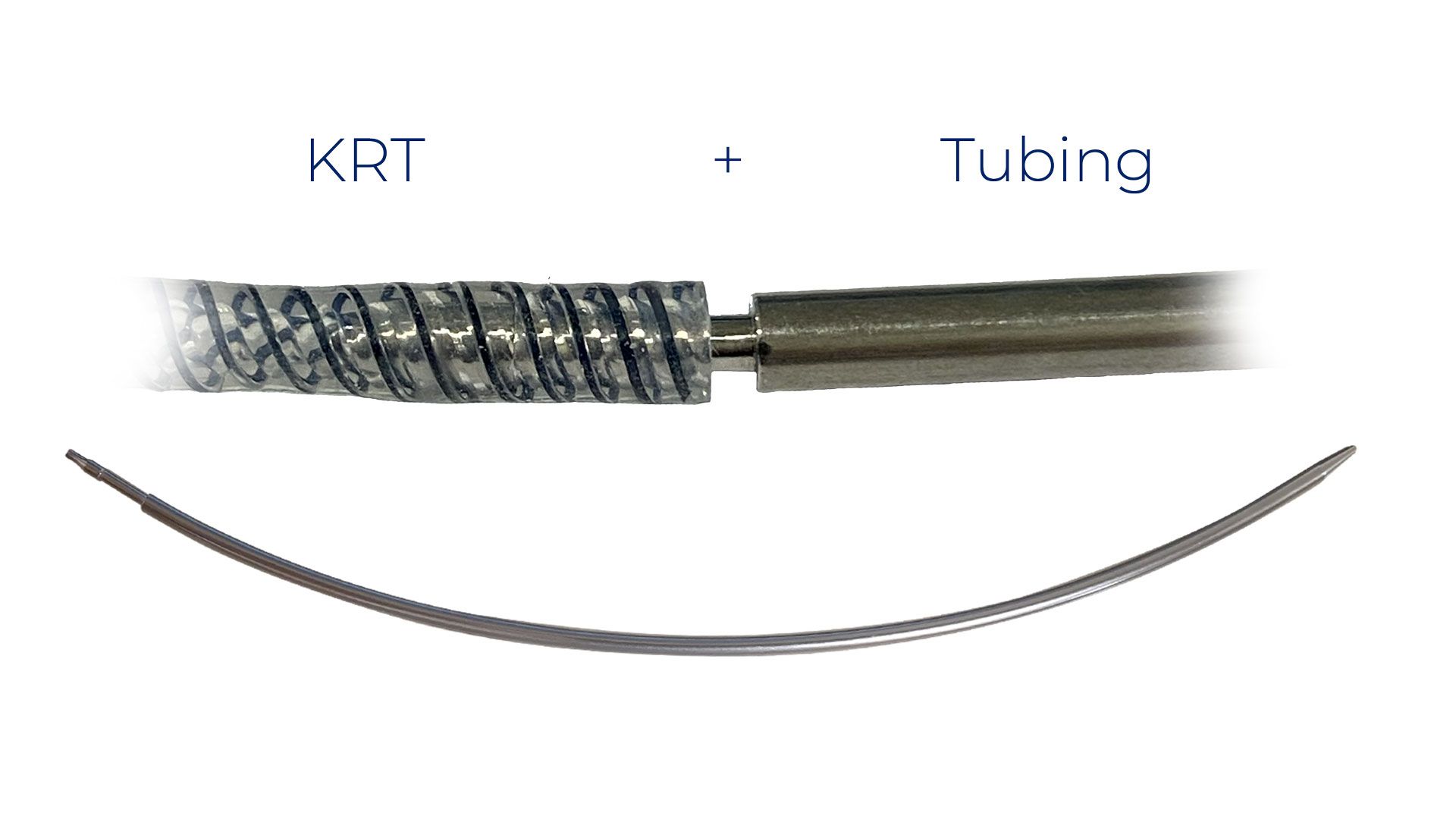
EasyClick™ Connector
EasyClick™ Connectors do not require an additional assembly tool.
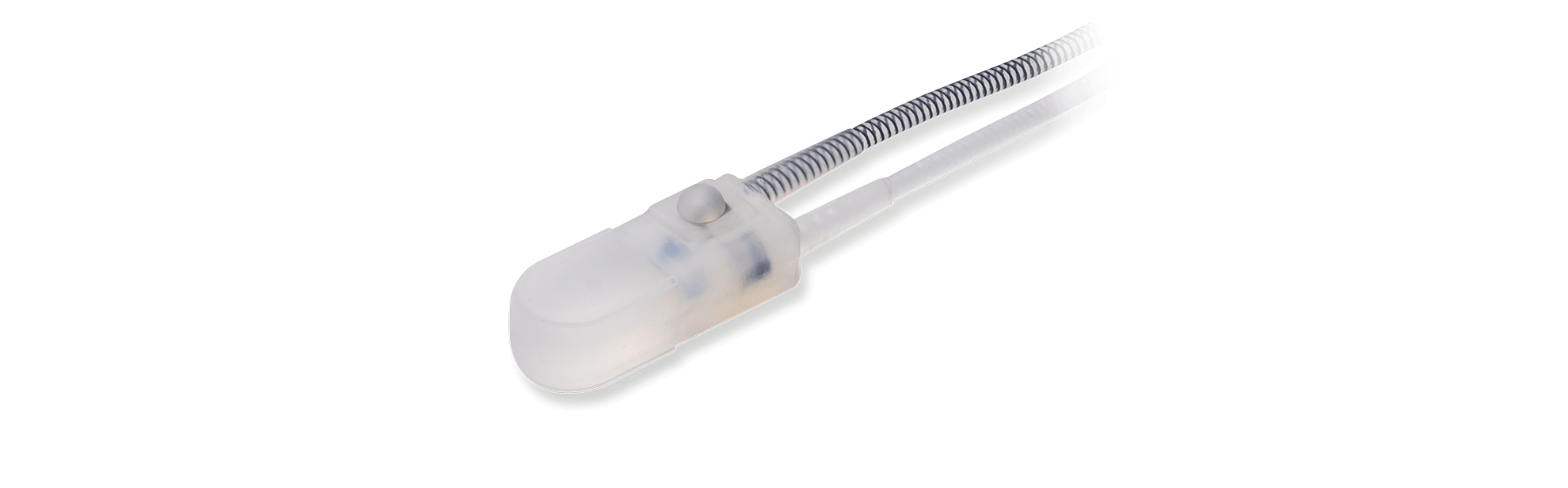
Control Pump
The ContiClassic® pump resembles competitive devices but differs because it is very easy to activate and deactivate.
While competitive pumps are difficult to turn on and turn off, this pump can easily be activated without the necessity of a large amount of fluid left in the pump. Ease of operation makes it possible to teach the patient to deactivate the pump when sleeping which protects his urethra from constant occlusion 24 hours, 7 days a week
ContiClassic® At A Glance
FAQ
What is urinary incontinence?
Urinary incontinence is the embarrassing loss of urine without the owner’s permission.
There are two types:
- Urgency incontinence which is when you have the sudden urge to urinate and cannot get to the toilet in time.
- Stress incontinence which is the loss of urine anytime there is an increase of abdominal pressure such as coughing, sneezing, changing position.
What is the common cause of stress incontinence in men?
Unlike women who can develop stress incontinence from simply having children or aging, men will only develop the condition after having some form of invasive pelvic surgery such as a prostatectomy for cancer. The surgery injures the urinary sphincter causing it to be unable to hold urine in the case of increased abdominal pressure.
Is stress incontinence a normal part of ageing?
Yes, it is true for women but not for men.
How do doctors diagnose urinary incontinence?
Generally, physicians rely upon a physical examination and a detailed medical history. If it is unclear whether the incontinence is urgency or stress, the physician may perform some testing.
Is stress urinary incontinence a side effect of surgical removal of the prostate?
Yes, particularly the radical prostatectomy for cancer has an increased incidence of this complication. In most men the incontinence persists for 3-6 months but resolves without treatment. If you are still leaking after 6 months, you should see a urologist who commonly treats male incontinence.
What are the treatment options for stress incontinence in men?
Unfortunately, there are very few non-surgical alternatives. Drugs and pelvic exercises, while effective in women, usually do not work in men with a damaged sphincter from a surgical procedure. There are two surgical treatments that have success: male sling and artificial urinary sphincter (AUS).
What is an artificial urinary sphincter (AUS)?
An AUS is a surgically implanted device to replace your damaged sphincter. It consists of a pump, cuff and pressure regulating balloon. It is implanted, generally as an outpatient, through a small incision in the scrotum or beneath the scrotum in the perineum. The surgery generally can be done in an hour and post-operative recovery is quick with minimal discomfort. The patient is not able to use the sphincter for 6 weeks to allow the tissues to heal. The device mimics the role of a healthy sphincter. The urethra remains closed until the bladder fills with urine and creates the need for emptying. The patient then squeezes the pump to open the urethra and allow the bladder to empty. Over the next two minutes the cuff gradually closes to allow the patient to regain continence.
What are the benefits of the ContiClassic® Artificial Urinary Sphincter?
Most patients who are incontinent are dry when sleeping because there are no increase of abdominal pressure events. Unlike competitive AUS, the ContiClassic® AUS is easily deactivated at night and turned back on the next morning. By allowing the urethra to rest during sleep without pressure, it is thought the need for revision surgery will be less. There are other improvements over existing competitive devices like more sophisticated control of cuff pressure during times of increased abdominal pressure, more sizes of cuff to allow more accurate sizing, and improved instrumentation for implantation of the device by your surgeon.